Returning to school with type 1 diabetes
Returning to school with Type 1 Diabetes includes more than shopping for new supplies and clothing.
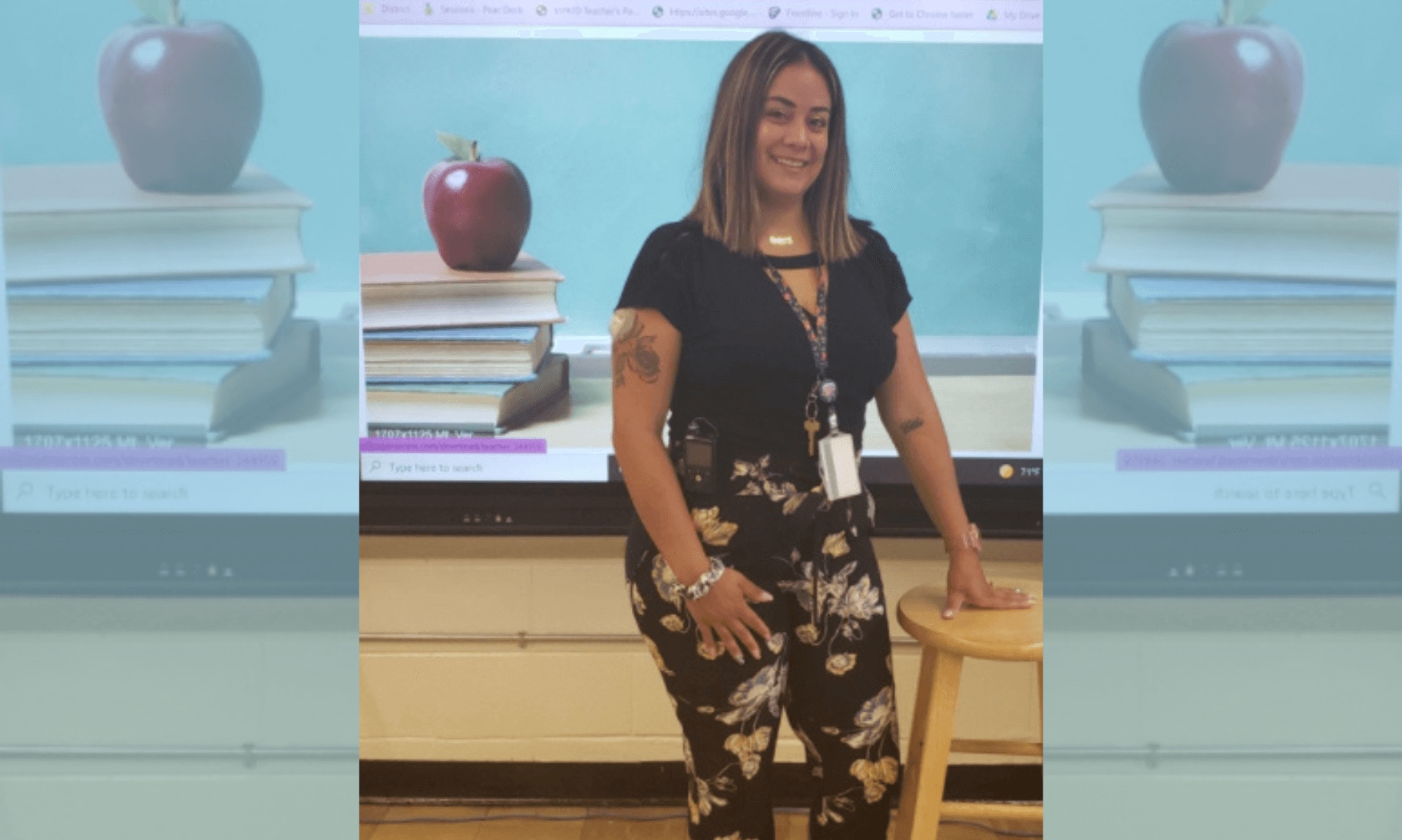
I have been a Special Educator for over 18 years, who lives with Type 1 Diabetes. My yearly experience on the first day of school has been lots of stares and questions regarding my CGM (Continuous Blood Glucose Monitor) and MiniMed™ 770G insulin pump. When I introduce myself I always go into a mini lesson/discussion regarding what Type 1 diabetes is and how amazing new technology helps me to manage my diabetes. I show my students all the different parts of my MiniMed™ 770G system. I share how I usually hide my actual pump somewhere beneath my clothing but I assure them that it is always connected to me.
Next, I show them how technology evolved and now I can see my sugar levels right on my cell phone. I explain at times they may hear alarms and that they all mean different things. I allow my students to ask me any questions they have and they always come up with great questions. Many of my students do research and share new things they learned about diabetes with me. I give the same presentation to my student’s parents during “Open House” parent night. I always make sure I stress the fact that I have never let Diabetes stop me from following my dream to become an educator or from doing ANYTHING in life!
From an educator's point of view, here are some important “Type 1 Tips for The Teacher,” to help ease parents, students and school faculty into the start of a new school year.
First, if a child has a plan in place such as an Individualized Education Plan, 504 accommodation plan or diabetes school plan parents should review these plans with their child’s teachers and nursing staff. A routine should be put into place for the exact time of day the child should report to the nurses office to check in, calibrations, fingersticks, boluses, etc. My previous students have always checked in with the nurse first thing in the morning, before lunch in order to bolus based on the carbohydrate to insulin ratio provided by the child’s doctor and before they headed on the bus to go home. Bus rides for students can be as long as 45 minutes long, therefore the bus driver should be included in your child’s plan. A plan for special occasion treats and class trips should also be discussed.
I think it is particularly important to sit down with your child’s teacher before the start of school and give an explanation of what type 1 diabetes actually is. In my everyday life I come across people who get type 2 and type 1 diabetes confused. Therefore a clear simple explanation could really help the school staff understand the seriousness of type 1 diabetes. Depending on your child's comfort level he or she may want to be discreet or share the fact that they have diabetes with their classmates. As I said before, I have always shared this with my students and their parents because some days they could see or hear my insulin pump. I have had students who share to avoid the stares and questions. I have also had students who chose to be discreet.
Next, you can provide teachers a list of warning signs of high blood sugars:
- Thirst
- Headaches
- Trouble concentrating
- Blurred vision
- Frequent urination
- Fatigue (weak, tired feeling)
As well as a list of warning sign of low blood sugars:
- Hunger
- Shakiness
- Anxiety
- Sweating
- Pale skin
- Fast or irregular heartbeat
- Sleepiness
- Dizziness
I have two posters with visuals and words describing both high and low blood sugar warning signs. My students always appreciate these posters year after year.
Lastly, make sure your child has back up supplies in the nurse's office. If your child is on an insulin pump, please pack extra batteries! (as well as pump supplies or insulin pen supplies). It can be easy to miss the warning alert for a low battery and find your child’s insulin pump has run out of power. Also think about keeping extra insulin on hand in the nurse’s office or an emergency contact of a person who is available to bring insulin to your child’s school in case of an emergency. Remember to keep a fully stocked (lancets and test strips) blood glucose meter in your child’s nurses office even if he or she is on a continuous glucose monitor. Preparation is key across the board for a successful school year!
The testimonial is of an individual’s experience using a Medtronic device. The opinions expressed in this blog do not take the place of medical advice or guidance. Please reach out to your healthcare team if you have for questions or concerns about your diabetes management.
IMPORTANT SAFETY INFORMATION MINIMED™ 770G SYSTEM WITH SMARTGUARD™ TECHNOLOGY
The MiniMed™ 770G system is intended for continuous delivery of basal insulin (at user selectable rates) and administration of insulin boluses (in user selectable amounts) for the management of type 1 diabetes mellitus in persons two years of age and older requiring insulin as well as for the continuous monitoring and trending of glucose levels in the fluid under the skin. The MiniMed™ 770G system includes SmartGuard™ technology, which can be programmed to automatically adjust delivery of basal insulin based on continuous glucose monitoring (CGM) sensor glucose (SG) values and can suspend delivery of insulin when the SG value falls below or is predicted to fall below predefined threshold values.
The Medtronic MiniMed™ 770G system consists of the following devices: MiniMed™ 770G insulin pump, the Guardian™ Link (3) transmitter, the Guardian™ Sensor (3), one-press serter, the Accu-Chek® Guide Link blood glucose meter, and the Accu-Chek® Guide test strips. The system requires a prescription.
The Guardian™ Sensor (3) has not been evaluated and is not intended to be used directly for making therapy adjustments, but rather to provide an indication of when a fingerstick may be required. All therapy adjustments should be based on measurements obtained using a blood glucose meter and not on values provided by the Guardian™ Sensor (3).
All therapy adjustments should be based on measurements obtained using the Accu-Chek® Guide Link blood glucose meter and not on values provided by the Guardian™ Sensor (3). Always check the pump display to ensure the glucose result shown agrees with the glucose results shown on the Accu-Chek® Guide Link blood glucose meter. Do not calibrate your CGM device or calculate a bolus using a blood glucose meter result taken from an Alternative Site. It is not recommended to calibrate your CGM device when sensor or blood glucose values are changing rapidly, e.g., following a meal or physical exercise.
WARNING: Do not use the SmartGuard™ Auto Mode for people who require less than 8 units or more than 250 units of total daily insulin per day. A total daily dose of at least 8 units, but no more than 250 units, is required to operate in SmartGuard™ Auto Mode. |



