The content on this page is informational only and does not take the place of medical advice or guidance. Please reach out to your healthcare team if you have questions or concerns about your diabetes management.
Symptoms of diabetes
Besides frequent urination, increased thirst, fatigue, and other issues, a person with diabetes can experience other symptoms and complications that can become serious. That’s why it’s important to keep blood glucose levels in a reasonable range.
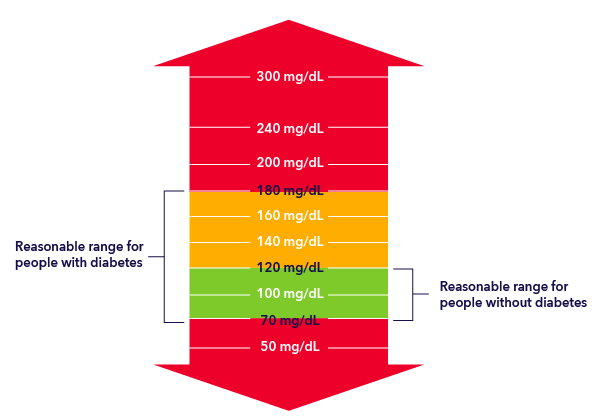
High and low glucose levels
A person who does not have diabetes usually has glucose levels from 70 mg/dL to 120 mg/dL. For those with diabetes, it is very difficult to keep glucose levels within such a tight range. A more reasonable range for people with diabetes is from 70 mg/dL to 180 mg/dL.
When glucose is too low
Hypoglycemia: Hypoglycemia, or “low blood sugar,” happens when someone doesn’t have enough glucose, or sugar, in their blood. For those with diabetes, it could be an indication that there is more insulin in the body than is needed.
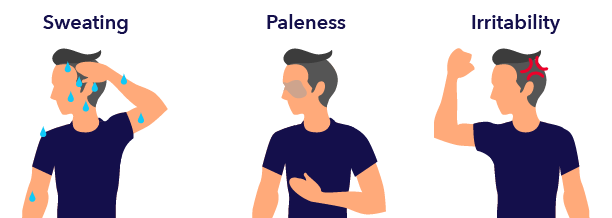
It is more than just being hungry. People experiencing hypoglycemia can start to feel shaky or experience other issues, including:
- Dizziness
- Sweating
- Anxiety
- Confusion
Untreated hypoglycemia can become very serious and lead to other issues, including convulsions or seizures, and sometimes even death.
Managing hypoglycemia: If someone is experiencing hypoglycemia, it’s important for them to eat or drink sugar to return glucose levels to normal. This can be in the form of hard candies, glucose tablets, juices, or sodas. Don’t forget that diet sodas, even though they taste sweet, do not have sugar in them.
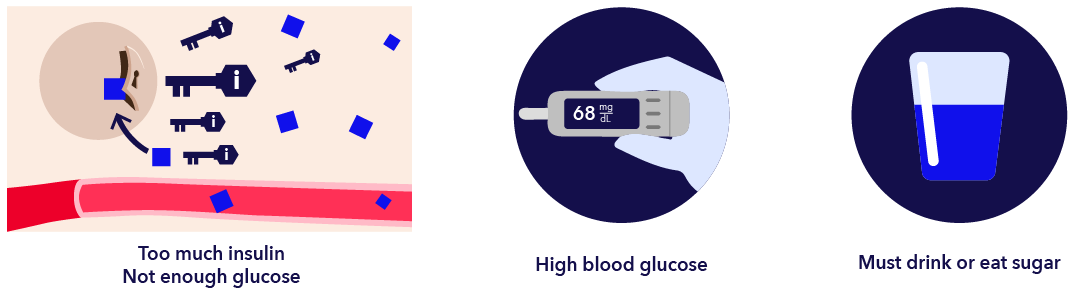
For those with diabetes, it’s important to not raise blood sugar levels too high. This can put them at risk of other, very serious complications.
When glucose is too high
Hyperglycemia: Hyperglycemia, or “high blood sugar,” happens when there is too much glucose in the blood. More insulin is needed to lower blood glucose levels.
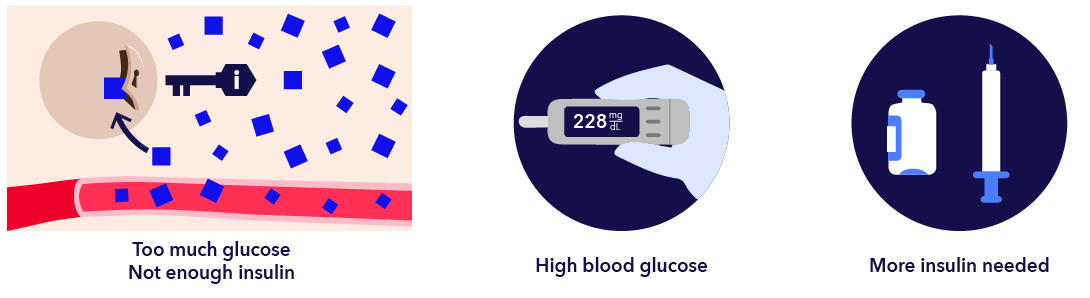
Too much blood glucose can lead to severe complications, so it’s important to keep levels in range.
Diabetic ketoacidosis (DKA) and ketones
When a body’s cells aren’t getting enough glucose, they start to burn fat for energy. When this happens, chemicals called ketones are released into the blood to break down the fat. These ketones turn the blood acidic, which is toxic at high levels.
DKA is a dangerous condition that often requires hospitalization. It can lead to diabetic coma or death. That’s why it’s important to watch for warning signs, such as:
- Extreme thirst
- High blood glucose levels
- Frequent urination
- Fruity or sweet breath
- Difficulty breathing
- Confusion
Skin problems
When blood glucose levels are not under control, people with diabetes can sometimes develop skin conditions, including:
- Patches of thickened skin
- Diabetic blisters on feet, hands, and other parts of the body
- Areas of darkened skin on face, armpits, and elsewhere
- Brownish patches on the shins
- Raised red spots that grow and turn yellowish
- Skin ulcers
- Waxy, pimply bumps
- Staph and fungal infections
Lumps and bumps
Sometimes people develop lumps and bumps called lipohypertrophy at insulin injection sites. These bumps can affect insulin absorption, so it’s important to always rotate the injection areas of the body.
Dawn phenomenon
People with diabetes sometimes awaken with elevated levels of glucose in their blood. This is called dawn phenomenon. It affects people with type 1 and type 2 diabetes.
To prevent dawn phenomenon, it’s important to work with a medical professional to help prevent or correct high morning glucose levels. This may include:
- Waking overnight to check insulin levels
- Using long-acting insulin injections later in the evening
- Adjusting insulin doses
- Avoiding bedtime snacking
- Using an insulin pump and continuous glucose monitor (CGM) to adjust insulin levels
Sick days
Having a flu or a cold can affect blood sugar levels and can raise the risk for of getting very ill. Experts recommend putting together a sick day plan with the healthcare team so people with diabetes are prepared ahead of time. This can include guidance on when they should call the doctor, how often to check blood sugar, additional symptoms to watch for, and perhaps preparing a kit of supplies to have on hand when illness strikes.
Healing bruised fingers
Frequent blood glucose testing using fingerstick tests can cause bruising. This can make it painful and difficult to test insulin levels. Using good fingerstick techniques, such as frequently changing lancets and rotating fingerstick sites, can help.
Foot health
High blood glucose levels can cause neuropathy, or nerve damage, in the feet (and sometimes in hands and arms). This nerve damage can cause pain, tingling, and numbness. The numbness can be dangerous because it makes it difficult to feel cuts, blisters, or ulcers (sores), which could get worse and become infected.
It’s important to check the feet every day for changes, blisters, or sores. And if neuropathy is present, it’s a good idea to always wear shoes to protect the feet.
Gastroparesis
People with type 1 or type 2 diabetes can sometimes experience a disorder called gastroparesis, which is also called delayed gastric emptying. This is when the nerves to the stomach are damaged and slow down the muscles and intestines, so food moves slowly or stops completely. This can make it harder to control blood glucose levels.
With gastroparesis, food that is stuck in the stomach can start to attract bacteria and ferment. This can be painful. Sometimes the food can become a solid mass called a bezoar. These can be dangerous if they block food from passing into the small intestine.
It’s important to watch for symptoms of gastroparesis, which can include:
- Nausea
- Vomiting
- Feeling full early in a meal
- Weight loss
- Bloating
- Lack of appetite
- Stomach spasms
Managing gastroparesis involves regaining control of blood glucose. In addition, it may require medications or dietary changes. Severe cases can sometimes require using a feeding tube, surgery, or other treatment.
Eye problems/diabetic retinopathy
Ongoing high blood sugar can lead to problems with vision.
Blurry vision: High blood sugar can cause the eye’s lenses to swell, making it difficult to see clearly.
Cataracts: Cloudy lenses can obscure vision. Anyone can get cataracts, but people with diabetes tend to get them earlier and sometimes worse than others.
Glaucoma: This happens when the eye doesn’t drain as it should, and pressure builds up. It can damage nerves and blood vessels. This can lead to changes in vision.
Neovascular glaucoma: This is a type of glaucoma that causes blood vessels to grow on the iris, or colored portion of the eye. They cause pressure to build up, which can cause damage.
Diabetic retinopathy: Diabetic retinopathy occurs when the blood vessels of the retina (the back of the eye that processes light) are damaged. If enough damage happens, it can lead to blindness. There are varying levels and types of this condition. It’s important to get yearly eye exams. If this condition is caught early, it can be slowed or prevented by controlling blood glucose levels.
Managing diabetes is an ongoing process and can be challenging. If you need support, remember Medtronic is here to help wherever you are along your journey.
Looking for more tips? Join the list
Subscribe to our newsletter, News to Infuse and receive monthly diabetes tips and helpful information.
1. National Institutes of Health. (n.d.). [Brochure]. Author. Retrieved from https://www.nei.nih.gov/sites/default/files/2019-06/diabetes-prevent-vision-loss.pdf