Lumps and bumps around insulin injection sites
Regular insulin therapy helps people with diabetes manage their blood sugar. But you may have noticed lumps or bumps on your skin around insulin injection sites. There’s no need to worry about this normal side effect of insulin therapy. Here are answers to some questions about these bumps and how you can avoid them.
What are the lumps and bumps at insulin injection sites?
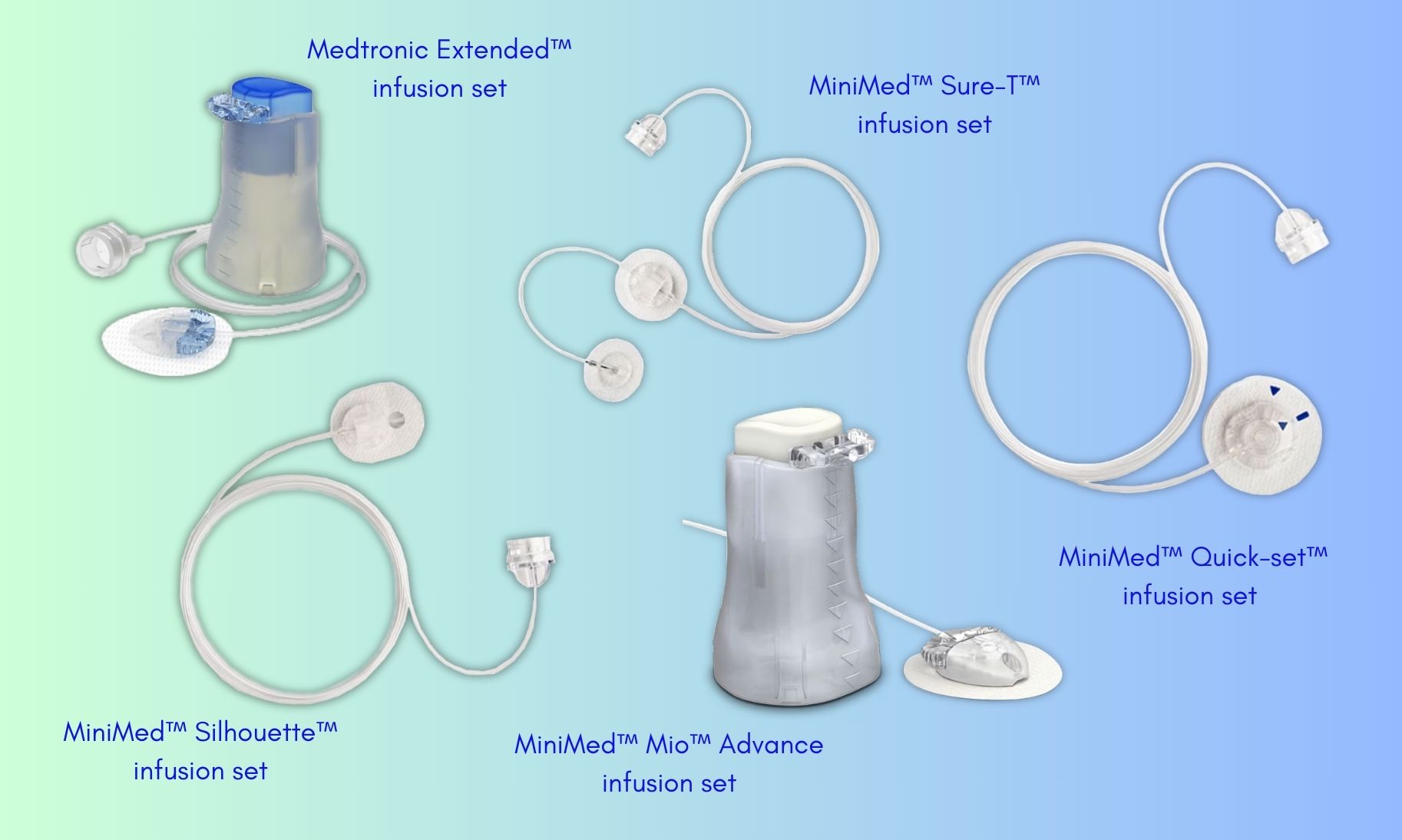
When fat cells come in contact with insulin, they can increase in size. If this happens in the same spot over and over again, you can develop lipohypertrophy. This is the medical term for a lump under the skin from a buildup of fat at the infusion or insulin injection site. Scar tissue, or hardened areas, may also develop at these sites. Easy-to-reach infusion and insulin injection sites (both sides of the belly button and on the sides of the thighs) are more prone to getting these lumps and bumps. Anyone who takes insulin can develop lipohypertrophy, whether they use a syringe or an insulin pump.
What happens with these lumps and bumps?
Developing lipohypertrophy can affect how well you can control your blood sugar with insulin. Affected areas don’t absorb insulin as well. In fact, as it progresses, the more likely it is that glucose control will be affected. Sometimes these areas have damaged nerve endings, leading to a loss of feeling, so you will not feel the needle going in at all. This is a sign you should stay away from that spot. As long as you stop using the affected site, lipohypertrophy should go away on its own in a matter of weeks or months.
How can you prevent lipohypertrophy if you need to take insulin?
If you tend to use the same spots repeatedly, you may want to use one of these approaches:
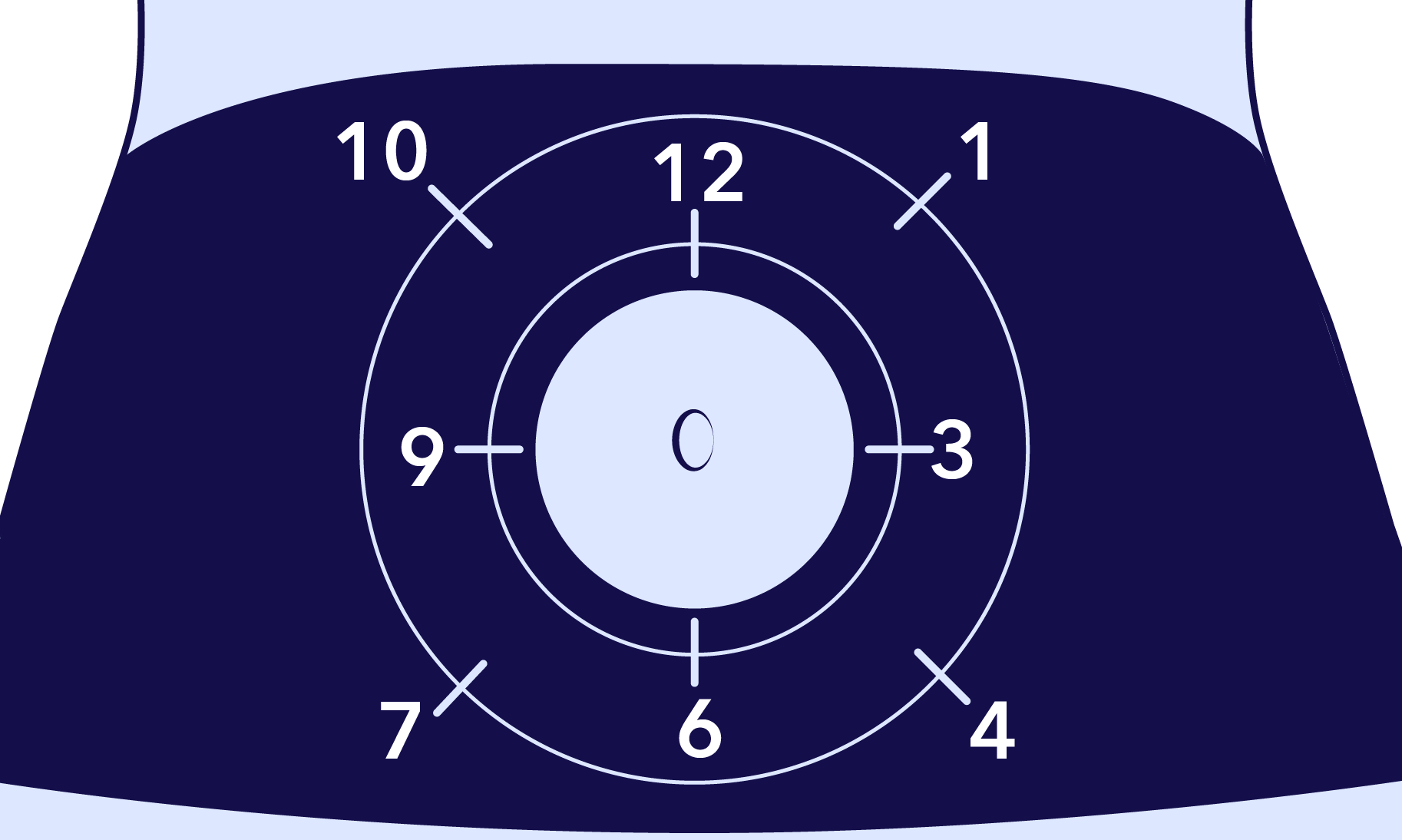
- Use a visual body map. Imagine a clock or the letters “M” or “W” on a body part like your abdomen. Trace your finger along this shape. The next time you poke your skin, try a different spot along this imaginary shape.
- Create your own simple method. Try this: if you insert a glucose sensor on the right side of your body, then do your next injection or next couple of infusion sets there, too. The next time you change your sensor and move it to the left side, insert your next couple infusion sets on the same side.
- Track sites with a calendar. On specific days of the week, you can do injections or infusion set insertions on the front side of your body while the other days could be reserved for the back. You can reserve certain times of the year for specific areas of your body, as well. You could try to wear infusion sets on the back of your arm when you’re more bundled up during the winter or your buttocks more often during swimsuit season. This will allow longer periods of time for tissue on other sites to heal, too.
- Talk to your doctor about new injection locations. There may be areas you haven’t thought of using to avoid lipohypertrophy. Just remember, any time you use a new area for injection or insertion sets, you may need to test your glucose more frequently since insulin will be absorbed differently. If you have been using your abdomen (where insulin is generally absorbed the fastest) and start using your buttocks (where insulin is absorbed more slowly), you may see your glucose values change more slowly.
Here's a guide of some potential areas to use during insulin therapy:

Before you inject insulin or insert a new infusion set, take a moment to firmly stroke the areas in a sweeping motion to feel for any lumps. If you find areas with lumps and bumps, allow them to heal before using them again. Healing time will vary, but you may want to wait at least a few weeks. We hope these tips help you as you continue to use insulin. Thanks for reading!
IMPORTANT SAFETY INFORMATION
-
Medtronic Diabetes insulin infusion pumps, continuous glucose monitoring systems and associated components are limited to sale by or on the order of a physician and should only be used under the direction of a healthcare professional familiar with the risks associated with the use of these systems.
-
Successful operation of the insulin infusion pumps and/or continuous glucose monitoring systems requires adequate vision and hearing to recognize alerts and alarms.
Medtronic Diabetes Insulin Infusion Pumps
-
Insulin pump therapy is not recommended for individuals who are unable or unwilling to perform a minimum of four blood glucose tests per day.
-
Insulin pumps use rapid-acting insulin. If your insulin delivery is interrupted for any reason, you must be prepared to replace the missed insulin immediately.
[Originally published 2012-01-17. Updated 2023-06-19]